Blog

What are the risks and complications associated with bariatric surgery (and how likely are you to keep the weight off)?
Things you should know and nutritional considerations
Bariatric surgery is the most successful method of weight loss that currently exists, and its ability to improve some chronic conditions is widely praised. However, the procedure may not be the miracle cure that you’ve been led to believe it is! This article will discuss some of the surgical risks and nutritional issues associated with bariatric surgery, as well as looking at the research around its long-term efficacy.
Bariatric surgery is a type of surgery designed to bring about weight loss. The first of its kind was performed in 1954, but weight loss surgery didn’t gain popularity with the wider public until the 1990s. In 2017-18, close to 7000 people in the UK underwent bariatric surgery.1 This statistic is much lower than in the US, for example, where 228,000 bariatric surgeries were performed in the same time period.
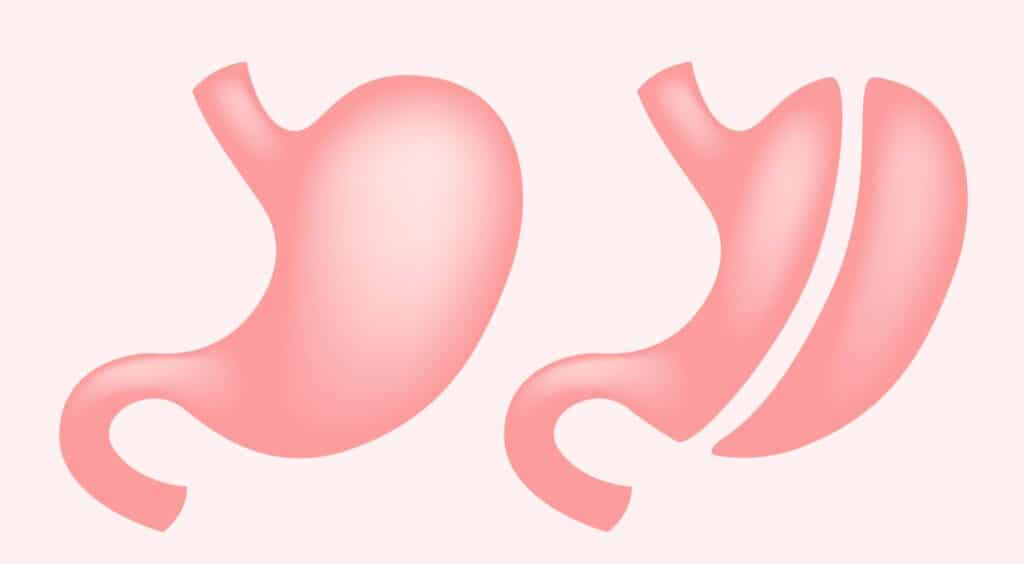
There are three different types of bariatric surgery that are commonly performed, which are intended to restrict the amount of food able to be consumed and/or the amount of nutrition able to be absorbed by the body.
ONE: Gastric band surgery (aka lap band)
In this procedure, an adjustable ring is placed around the top part of the stomach to constrict it, causing the patient to feel fuller more quickly. This surgery makes up 10% of bariatric procedures.2
TWO: Gastric bypass surgery (aka Roux-en-Y)
In this surgery, a small section of the stomach is isolated with staples and then attached directly to a lower part of the small intestine. By doing this, the patient feels full more quickly and absorbs less of the nutrients from the food consumed. Unlike gastric band surgery, gastric bypass surgery is irreversible and has a longer recovery period. This procedure makes up 45% of bariatric surgeries.2
THREE: Gastric sleeve surgery (aka sleeve gastrectomy)
In a gastric sleeve surgery, around three-quarters of the stomach is removed, significantly reducing the amount of food that can be consumed. Additionally, the production of ghrelin (the hunger hormone) is suppressed, causing a reduction in appetite. This procedure is irreversible and makes up 37% of bariatric surgeries.2
A fourth procedure known as a biliopancreatic diversion also exists, but is rarely used (less than 2% of the time) due to its high risk of nutritional complications.2 More information about types of bariatric surgery can be found on the NHS website.
What are the surgical risks and complications associated with bariatric surgery?
An ongoing study funded by the US government has found that one in every 25 bariatric patients experience a serious complication as a result of their surgery.3 Three in every 1000 bariatric surgeries result in death.
Immediate risks associated with the surgery itself are excessive bleeding, infection, blood clots, respiratory issues and leaking in the gut.
Long-term complications vary depending on the type of procedure. For example, common complications associated with gastric banding are infection, erosion and slippage of the band, whereas dumping syndrome is common following gastric bypass.
In some cases, there is a need for a second surgery to correct severe side effects or complications. Revisional surgeries tend to be riskier than the primary procedure, with more the death rate increasing five-fold.4 Revisions are most common in gastric banding surgery, with up to 50% of patients requiring a second operation.4
What are the nutritional issues caused by bariatric surgery?
Lifelong monitoring and a long-term “bariatric diet” is required to manage nutritional complications following bariatric surgery – some of which may be life threatening.
Eating too quickly, consuming portions of food that are “too large” or having liquids too close to eating are known to cause symptoms like regurgitation, vomiting, reflux or a build-up of saliva.
Dehydration is significant concern for bariatric patients as it is the principal cause of re-hospitalisation after surgery. It is also known to increase nausea, in conjunction with post-op medication side effects. However, there are several restrictions in place when it comes to the intake of liquids – primarily the ongoing avoidance of all carbonated and alcoholic drinks, as well as avoiding drinking fluids with meals or for 30 minutes following. As such, it is extremely important to sip on water throughout the day following bariatric surgery, in order to maintain hydration.
Nutrient deficiency is another concerning complication of bariatric surgery.
Thiamine (aka vitamin B1)
Patients with gastric banding, or who are experiencing ongoing vomiting, are at particular risk of thiamine deficiency. It’s fairly uncommon in the general population and so you may not have heard of it before! Untreated, thiamine deficiency can have permanent and devastating effects on the heart and brain. Consequently, it is incredibly important to be vigilant in taking supplements as recommended by your health provider – this is generally a lifelong requirement. Additionally, thiamine can be found in foods like pork, fish, nuts, and wholegrains.
Vitamin B12
Adequate stomach acid is needed to release vitamin B12 from food in order for it to be absorbed by the body. This is a particular issue for gastric bypass patients, who experience a significant reduction in stomach acid production as a result of their procedure, leading to up to a quarter of patients being deficient in this vitamin.5 B12 deficiency can cause reduced mobility, neurological disturbances and psychiatric symptoms, but can be avoided with supplementation and a diet rich in foods like meat, fish, poultry and dairy.
Calcium/Vitamin D
You probably know that calcium is essential for bone health, but did you know that adequate vitamin D is needed to absorb calcium from food? Vitamin D deficiency occurs in up to 80% of bariatric patients, so it’s probably no surprise that there is an increased risk of bone fractures in this population.6 Dairy and leafy green vegetables are excellent sources of calcium, while the sun is our best-known source of vitamin D. Supplementation is also often recommended to make sure you’re meeting your requirements.
Protein
Lastly (and arguably most importantly), protein malnutrition is a significant risk for bariatric patients and is mainly caused by ongoing vomiting or an inadequate intake of protein-rich food. Long term, protein malnutrition can cause muscle wasting, hair loss, fatigue and weakness. Requirements for protein are significantly higher after bariatric surgery – up to twice the recommendation for the general population – and it can be incredibly difficult to eat enough protein-rich foods when appetite is so severely suppressed.7 You might be recommended a protein supplement to counteract this by your health provider.
How effective is bariatric surgery in the long term?
While bariatric surgery is the most effective method of long-term weight loss, it’s certainly not perfect. In the ten years following surgery, most bariatric patients regain around quarter of the weight they initially lost.8 A small number of patients (around four in every 100) will regain all of the weight they lost, and sometimes more.9
There are a few reasons as to why bariatric surgery is not always effective in the long-term.
Firstly, the maintenance of lean body mass uses more energy (aka calories) than fat mass. In other words, the greater your muscle mass, the greater the amount of energy you use just to stay alive. Along with its intended result of reduced fat mass, bariatric surgery also causes a significant loss of muscle mass, which is thought to contribute in part to the rates of weight regain.
Additionally, reduced intake of calories is another intended consequence of bariatric surgery. However, ongoing calorie restriction causes metabolism to slow as a survival mechanism, in order to prevent starvation. The slower a person’s metabolism, the more efficient their use of energy. This results in excess calories being stored as fat, contributing to weight regain.
If you’re interested in learning more about how the body counteracts calorie restriction, check out our blog article about why dieting doesn’t work.
To summarise, while bariatric surgery certainly has its benefits, it also has its downfalls – mainly the significant risk of surgical complications, the high likelihood of nutritional deficiency and the strong probability of weight regain.
With all of this being said, our team here at Embody Health London are strong proponents of body autonomy, meaning we support your right to make decisions about your health based on what you feel is best. While we don’t encourage bariatric surgery, we DO support our clients no matter their decisions.
To learn more about how we can support you towards finding body peace and food freedom, reach out to us at [email protected].
Karli Battaglia MDiet, APD
EHL Team x
References
- National Health Service. Statistics on Obesity, Physical Activity and Diet. England: NHS Digital; 2019.
- Angrisani L, Santonicola A, Iovino P, Formisano G, Buchwald H, Scopinaro N. Bariatric Surgery Worldwide 2013. Obesity Surgery. 2015;25(10):1822-1832.
- Belle S, Berk P, Chapman W, Christian N, Courcoulas A, Dakin G et al. Baseline characteristics of participants in the Longitudinal Assessment of Bariatric Surgery-2 (LABS-2) study. Surgery for Obesity and Related Diseases. 2013;9(6):926-935.
- Ma I, Madura J 2nd. Gastrointestinal Complications After Bariatric Surgery. Gastroenterol Hepatol (N Y). 2015;11(8):526-35.
- Himpens J, Dapri G, Cadière G. A Prospective Randomized Study Between Laparoscopic Gastric Banding and Laparoscopic Isolated Sleeve Gastrectomy: Results after 1 and 3 Years. Obesity Surgery. 2006;16(11):1450-1456.
- Lupoli R, Lembo E, Saldalamacchia G, Avola C, Angrisani L, Capaldo B. Bariatric surgery and long-term nutritional issues. World Journal of Diabetes. 2017;8(11):464.
- Richardson W, Plaisance A, Periou L, Buquoi J, Tillery D. Long-term Management of Patients After Weight Loss Surgery. Ochsner J. 2009;9(3):154-9.
- Heber D, Greenway F, Kaplan L, Livingston E, Salvador J, Still C. Endocrine and Nutritional Management of the Post-Bariatric Surgery Patient: An Endocrine Society Clinical Practice Guideline. The Journal of Clinical Endocrinology & Metabolism. 2010;95(11):4823-4843.
- Maciejewski M, Arterburn D, Van Scoyoc L, Smith V, Yancy W, Weidenbacher H et al. Bariatric Surgery and Long-term Durability of Weight Loss. JAMA Surgery. 2016;151(11):1046.