Three ways to improve your gut health
The topic of gut health continues to spark interest with each day as research increasingly unveils more about the relationship between our gut and brain.
Our gut microbiota weighs as much as our brain itself, containing over 100 times more genes than those that make us human. All of this is fascinating within itself, but there is increasing insight into our gut also evoking symptoms of conditions such as depression, anxiety, autism and even Parkinson’s. (1)
Research has shown a strong relationship between mental health outcomes and gut symptoms such as indigestion, heartburn, acid reflux, constipation, diarrhoea, bloating, and other forms of pain and discomfort. (2)
This manifestation of our mental stress and emotions presenting as gut symptoms impacts our lives more than we once thought. As a result, researchers are already beginning to think about the potential use of bacteria in improving our mood and emotional wellbeing. In this article, you can learn more about this connection and how to optimise your lifestyle for a happier gut.
What actually is the gut?
The gut makes up part of our gastrointestinal (GI) tract, including our mouth, oesophagus (windpipe), stomach, small intestine, large intestine, and rectum. When we talk about the gut, we mostly mean the organs in the general stomach area, such as the intestines. The majority of consumed nutrients absorb into our bloodstream via the small intestine, where bacteria, fungi, algae and other populations, synergistically referred to as the microbiome, co-exist and interact. A highly diverse and well-fed microbiome is essential for efficient cognitive and emotional function. (3)
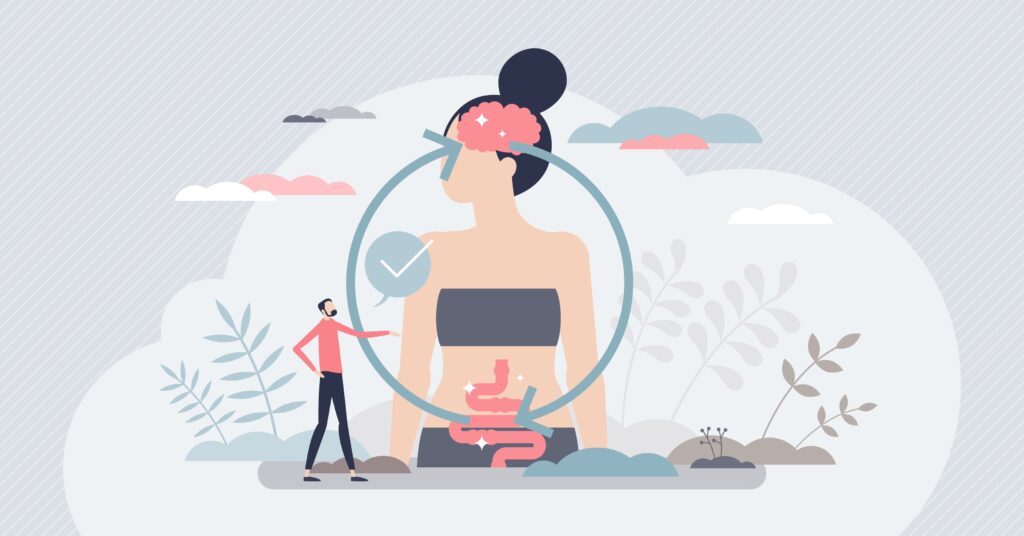
What is the gut-brain axis?
The gut-brain axis is the mechanism by which the gut communicates to the brain and vice versa. This primarily happens via the vagus nerve, a major nerve and component of the spinal cord that connects several organs in the body, including the heart and lungs. The vagus nerve makes up part of the sympathetic nervous system (SNS) and the parasympathetic nervous system (PNS), also known respectively as the ‘fight or flight’ and ‘rest and digest’ responses. (4)
The vagus nerve can help signal to surface receptors on cell membranes in the GI tract, such as the ones lining the intestines, stomach and pancreas. These cells can then respond and adapt to any changes through hormone secretion and can then react to any chemical, thermal or mechanical stimuli by sending signals up the vagus nerve back to the brain.
The brain can respond to these signals by altering the gut’s permeability or by inducing secretions and other hormones. And did you know there are five times as many nerve cells or neurones in our gut as there are in the entire brain and spinal cord – indicating the incredible sensitivity and susceptibility to change!
When we are in a stressed state, blood flow to the gut is reduced, and a ‘fight or flight’ response is sent via the SNS. The body’s digestive system then becomes repressed and deprioritised, failing to work at an optimum level. This is when gut symptoms may manifest in a variety of ways – including constipation, bloating, gas or diarrhoea. (4)
How can I alleviate my gut symptoms?
It is key to remember that gut symptoms may present very differently amongst individuals. Shorter-term stress may suppress our digestion, causing a reduction in appetite signals. In the long term, chronic stress may present as IBS or other GI disorders. Be sure to stay mindful of how symptoms may manifest for you and incorporate tools and support that you find most effective to help optimise your quality of life.
ONE: Journalling
It may be beneficial to reflect on patterns in gut symptoms and your mood using tools such as journalling or starting a food and mood journal. Having this on paper can help you to look for potential triggers and may help you in finding the source of problematic symptoms. As mentioned earlier, gut symptoms can be enhanced by stressful factors and not just what we consume – so noticing your mood and feeling changes throughout the day can be invaluable.
TWO: Yoga and gentle movement
The ancient science of yoga and mindfulness can act as a gentle form of movement, helping to reduce stress levels and also aid gut motility in the body. (5) Taking time out of your day to complete a sequence of postures can ease discomfort – particularly the wind-relieving pose, spinal twists, and child’s pose. You can try this before a meal as well as when experiencing symptoms to relax the body and ease digestion. Use mindfulness to empower yourself through gut symptoms, and read about the mental rewards of yoga on our blog.
THREE: Nutrition
Fermented foods have been dated back to 7000 BC as a use in the human diet. (6) Incorporating probiotics and prebiotics into your diet may be effective in improving symptoms. You could experiment with drinks such as kefir or kombucha and foods including sauerkraut, kimchi, and tempeh. It may be helpful to be open, trying a range of products to find which are practical and enjoyable for you. Mixing varieties of these products can also be an excellent way to add variation and balance to your diet, as bacterial strains may vary between brands.
It is important to remember that many probiotic products still lack research. We do not always know if the bacteria obtained from them will survive our gut passage into the intestines, where it is at its highest population, so keep this in mind, as some products can be quite expensive. You can ask a registered dietitian or nutritionist interested in gut health to help you decide which may be a good fit for you if unsure.
In addition to probiotics, you may also want to opt for food high in prebiotics. Prebiotic foods are ones that pass through our GI tract, feeding our gut bacteria and enabling them to function optimally. High prebiotic foods include bananas, onions, garlic, asparagus, and Jerusalem artichoke.
Prebiotics are most beneficial when consumed on a regular, long-term basis as opposed to all at once or when experiencing uncomfortable symptoms, so it can be best to incorporate these into your diet more often.
Remember that you do not need to have a diagnosis of a gut issue in order to seek help and relief for your gut issues. Your personal symptoms and experiences are valid and deserve recognition whether you have an official diagnosis or not.
If you are feeling any of the below symptoms, do seek urgent medical care as this may be the sign of something more serious:
- Unexplained weight loss
- Severe pain or tenderness
- Blood in your stools or bloody diarrhoea
- Gut symptoms combined with shortness of breath, noticeable heartbeats or pale skin
- A hard lump or swell in your stomach
Many medications can also cause gut-related symptoms, so be aware of this happening when taking anything new.
Please speak to a dietitian, GP, or pharmacist who may be able to steer you towards practical ways to manage your symptoms.
We understand it can sometimes take a lot of strength, even just to get through the day, and we wanted to take this moment to remind you to always be kind to your body as it heals and grows through life. We are SO proud of you and here for you every step of the way!
Priya Chotai, BSc ANutr
EHL Team x
References:
1.Mussell, M, et al. Gastrointestinal symptoms in primary care: prevalence and association with depression and anxiety. (2008). Journal of Psychosomatic Research. 64(6): 605-612.
2. Posserud I, Agerforz P, Ekman R, Björnsson ES, Abrahamsson H, Simrén M. Altered visceral perceptual and neuroendocrine response in patients with irritable bowel syndrome during mental stress. (2004). Gut. Aug 1;53(8):1102-8.
3. NHS (2021) What is IBS? Irritable bowel syndrome (IBS), Available at: https://www.nhs.uk/conditions/irritable-bowel-syndrome-ibs/
4. Hall, John E. (2011). “General Principles of Gastrointestinal Function”. Guyton and Hal Textbook of Medical Physiology(12th ed.). Saunders Elsevier. p. 755. ISBN978-1416045748
5. Black, D.S., Slavich, G.M. (2016) ‘Mindfulness meditation and the immune system: a systematic review of randomised controlled trials’, Annals of the New York Academy of Sciences, 373(1), pp. 13-24.
6. Maicas, Sergi. 2020. “The Role of Yeasts in Fermentation Processes” Microorganisms8, no. 8: 1142. https://doi.org/10.3390/microorganisms8081142